Patients Information :


 Laparoscopy and hysteroscopy:
Laparoscopy and hysteroscopy:
What is laparoscopy?
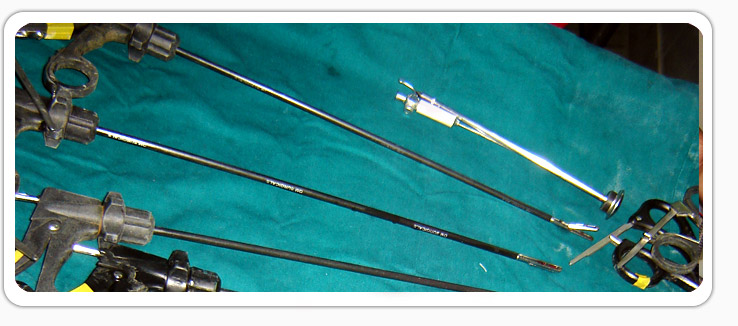
Laparoscopy is a surgical procedure performed through very small incisions in the abdomen, using specialised instruments. The abdominal cavity is inflated with carbon dioxide gas (CO2) and distended. A pencil-thin instrument called a laparoscope is used; it has lenses like a telescope to magnify body structures, a powerful light to illuminate them, and a miniature video camera. The camera sends images of the inside of the body to a TV monitor in the operating room. Specialised surgical instruments can be inserted through the small incisions nearby. This type of surgery is called 'minimal access' because of the very small incisions used. Yet major procedures can now be performed using this technique.What is hysteroscopy?
Diagnostic hysteroscopy is used to look inside the uterus. If an abnormal condition is detected during the diagnostic procedure, operative hysteroscopy can often be performed to correct it at the same time, avoiding the need for a second surgery.
What are the advantages of laparoscopy?
Laparoscopy is easier on the patient because it uses a few very small incisions. For example, traditional "open surgery" on the abdomen usually requires a ten to fifteen centimetre incision through layers of skin and muscle. In laparoscopic surgery, the doctor usually makes two to three incisions that are less than a centimetre long.
The smaller incisions cause less damage to body tissue, organs, and muscles so that the patient.
Laparoscopy for diagnosis and treatment.
Laparoscopy can be used either to diagnose or to treat various conditions. Or it may be used to identify a problem and treat it in the same operation.
What kinds of surgery can be performed with minimally invasive methods?
Dozens of different kinds of operations are now being done using these new minimally invasive techniques. Gynecological conditions or procedures which can be performed endoscopically include:
Is it possible to have my uterus, big fibroids or cysts removed through these tiny incisions? How is that possible?
Yes, even a very large uterus or large fibroids can be removed laparoscopically. The tissue to be removed is cut into pieces with specially designed- for this purpose-instrument. Then the pieces are removed through one of the incisions.
What are the possible risks of laparoscopy?
Since laparoscopy involves minimal damage to body tissues, it is generally safer than open operations. A complication is an unforeseen problem that occurs during or after surgery, such as internal bleeding or injury to a healthy organ.
Possible Complications of Laparoscopy
How can I pick the best doctor for minimally invasive surgery?
What kind of anesthesia is used for laparoscopy?
For laparoscopy, the patient is usually given a general anesthesia and is unconscious during the operation. General anesthesia relaxes muscles and makes it easier for the doctor to perform the surgery. Some procedures however are done with a local anesthetic.
Preparing for a Laparoscopy
Individuals scheduled for laparoscopy usually visit the hospital before the operation for preoperative evaluation and to discuss the procedure in detail. Tests may be ordered, which include blood and urine tests, an electrocardiogram, an ultrasound scan and a x-ray.
The Operation
The procedure depends on several factors, including the area of the body, the disease, the patient's condition, and whether the operation is to diagnose or treat
How Long Does Laparoscopy Take?
Diagnostic laparoscopy usually takes less than half an hour. If the procedure is for treatment, it will depend on the condition and the complexity of the operation. It may take an hour or more and sometimes much longer, depending on the procedure.
What Happens When The Patient Wakes Up?
The effects of general anesthesia make most people feel groggy at first, but they quickly become more alert. Some people experience nausea for a short time after awakening from a general anesthesia. In the recovery room, the individual first rests in bed, then gradually sits up, stands, and walks as balance and mobility are regained.
What Problems Can Occur After Surgery?
Complications after laparoscopic surgery are rare. Most people recover quickly and resume their normal activities without problems. However, the risk of infection or other problems exists as with any kind of surgery.
There may be discomfort in the abdomen, upper chest, shoulders, and neck area due to the carbon dioxide used to inflate the abdomen, but this disappears quickly
Endometriosis:
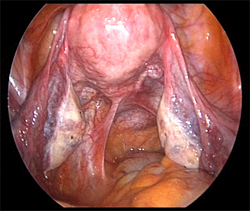
 Endometriosis is a condition where tissue similar to the lining of the uterus (which should only be located inside the uterus) is found elsewhere in the body.
Endometriosis is a condition where tissue similar to the lining of the uterus (which should only be located inside the uterus) is found elsewhere in the body.
Endometriosis lesions can be found anywhere in the pelvic cavity: on the ovaries, the fallopian tubes, and on the pelvic sidewall. Other common sites include the uterosacral ligaments, the cul-de-sac, the pouch of Douglas, and in the recto-vaginal septum.
In addition, it can be found in caesarian-section scars, laparoscopy or laparotomy scars, and on the bladder, bowel, intestines, colon, appendix, and rectum.
The most common symptom of endometriosis is pelvic pain. The pain often correlates to the menstrual cycle, but a woman with endometriosis may also experience pain that doesn’t correlate to her cycle. For many women, the pain of endometriosis is so severe and debilitating that it impacts their lives in significant ways.
Endometriosis can also cause scar tissue and adhesions to develop that can distort a woman’s internal anatomy. In advanced stages, internal organs may fuse together, causing a condition known as a "frozen pelvis."
It is estimated that 30-40% of women with endometriosis are infertile.
Symptoms of endometriosis
The most common symptom of endometriosis is pelvic pain. The pain often correlates to the menstrual cycle, however a woman with endometriosis may also experience pain at other times during her monthly cycle.
For many women, but not everyone, the pain of endometriosis can unfortunately be so severe and debilitating that it impacts on her life significant ways.
Pain may be felt:
Other symptoms may include:
The other well known symptom associated with endometriosis is infertility. It is estimated that 30-40% of women with endometriosis are sub fertile.
What causes endometriosis?
Several different hypotheses have been put forward as to what causes endometriosis. Unfortunately, none of these theories have ever been entirely proven, nor do they fully explain all the mechanisms associated with the development of the disease. Thus, the cause of endometriosis remains unknown.
Diagnosing endometriosis
There is no simple test that can be used to diagnose endometriosis. In fact, the only reliable way to definitively diagnose endometriosis is by performing a laparoscopy and to take a biopsy of the tissue. This is what is known as "the gold standard".
However, this is an expensive, invasive procedure. Furthermore, if the surgeon is not a specialist in endometriosis she may not recognise the disease, which can result in a "negative" diagnosis.
In addition, the woman/girl may not want to have surgery.
This makes diagnosis a challenge, and therefore an experienced gynaecologist should be able to recognize symptoms suggestive of endometriosis through talking with the woman/girl and obtain a history of her symptoms. For this to be effective, it is important that the woman/girl is honest with her physician about all of her symptoms and the pattern of these.
There are other tests, which the gynaecologist may perform. These include ultrasound, MRI scans, and gynaecological examinations. None of these can definitively confirm endometriosis (though they can be suggestive of the disease), nor can they definitively dismiss the presence of endometriotic lesions/cysts.
The fact that there is no non-invasive, definitive diagnostic method for endometriosis is as frustrating for clinicians as it is for women with the disease.
Treatments for endometriosis
Since the cause of endometriosis remains unknown, a treatment which fully cures endometriosis has yet to be developed.
Choosing a treatment therefore comes down to the individual woman's wishes, depending on her symptoms, her age, and her fertility wishes. She should discuss these with her physician so that they, together, can determine which long term, holistic, treatment plan is best for her individual needs. For many women, this can be a combination of more than one treatment.
Uterine Fibroids:
Introduction:
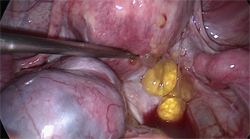
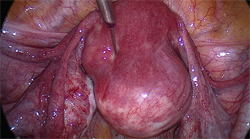
 Uterine fibroids are benign (noncancerous) masses of muscle tissue that enlarge and/or distort the uterus and sometimes the cervix. Fibroids originate from the smooth muscle cells within the myometrium or wall of the uterus. In most cases there are multiple fibroids, but occasionally a single fibroid may occur. Other terms for uterine fibroids are myomas or leiomyoma.
Uterine fibroids are benign (noncancerous) masses of muscle tissue that enlarge and/or distort the uterus and sometimes the cervix. Fibroids originate from the smooth muscle cells within the myometrium or wall of the uterus. In most cases there are multiple fibroids, but occasionally a single fibroid may occur. Other terms for uterine fibroids are myomas or leiomyoma.
It is estimated that uterine fibroids occur in one out of every four to five American women. African American women are over three times more likely to develop fibroids than Caucasian women. Usually, fibroids develop when a woman is in her 30s or 40s, and become smaller after menopause. Most fibroids do not require treatment. However, they may cause excessive uterine bleeding, pain, abnormal pressure sensations, and, less commonly, infertility, miscarriage, and premature delivery. Removing the fibroids surgically can usually correct these problems. However, there is a chance that additional fibroids and/or postoperative scarring will occur.
Cause:
Increased Estrogen Levels
The exact cause of uterine fibroids is unclear, but there is evidence suggesting that they require estrogen for growth. For example, fibroids some times grow larger during pregnancy when the body produces more estrogen.
During menopause when estrogen levels decline, fibroid growth generally subsides. Consequently, fibroids rarely require treatment after menopause.
Types of Fibroids:
Fibroids are usually found in or around the uterus, but they sometimes occur in the cervix. Fibroids can be divided into three categories: subserous, intramural, or submucous. Subserous fibroids are located in the outer wall of the uterus. Intramural fibroids are found in the muscular layers of the uterine wall, and submucous fibroids are located on the inner wall of the uterus and may protrude into the cavity. About 55 percent of fibroids are subserosal; 40 percent are intramural; and 5 percent are submucosal.
Symptoms:
Many women with uterine fibroids have no symptoms. However, approximately one-third report abnormal uterine bleeding, a feeling of pressure or pain in the pelvic or lower abdomen, or the presence of a mass. As fibroids enlarge and grow, the mass can become very large. Some women notice that their abdomen is larger and their clothes are tighter. Others can feel something protruding from the lower abdomen.
Abnormal Uterine Bleeding:
Abnormal uterine bleeding is most common symptom associated with fibroids and is present in one-third to one-half of women undergoing fibroid-related surgery. Large fibroids can distort or enlarge the uterine cavity, and this creates a larger surface area for menstrual bleeding. Fibroids also put pressure on the endometrium and cause excessive bleeding. Because abnormal uterine bleeding can result from other causes, such as endometrial cancer and hormonal problems, it is important that women experiencing abnormal vaginal bleeding receive a thorough evaluation, even if uterine fibroids are present.
Pain
When a fibroid begins to grow rapidly, it may outgrow its blood supply and degenerate or decay, causing a painful, cramping sensation. This most often happens during pregnancy. When sudden, severe pain occurs, it can sometimes be caused by decaying, inflamed, or twisting fibroids. Large and bulky uterine fibroids may make intercourse painful.
Pressure Symptoms
Large fibroids may produce pressure on various pelvic organs such as the bladder, ureters, and rectum. Consequently, urinary frequency or urgency may occur because of decreased bladder capacity. Continued compression of these organs can also cause kidney damage if the fibroids are not removed. Fibroids in the lower uterus may put pressure on the large bowel and rectum, which could result in difficult bowel movements, constipation, or hemorrhoids.
Fibroids and Infertility
Fibroids may contribute to an infertility problem. Most often, submucosal or intramural fibroids inside the uterus are associated with infertility. However, only 2 to 3 percent of infertile women are unable to conceive due to uterine fibroids. Because of this, women and their partners should have a thorough infertility investigation to identify additional causes of fertility problems.
Infertility may result from uterine fibroids for several reasons. Changes in the endometrium may make it unlikely for a fertilized egg to attach to the uterine wall. In addition, one or both fallopian tubes may be compressed or blocked, thus preventing the sperm from reaching the egg. Conception rates after any of the surgical techniques (myomectomy) used to remove fibroids are generally good but depend upon other factors that influence fertility such as age, previous pregnancy, ovulatory status, the status of the fallopian tubes, and the male’s semen quality. Fibroids may increase miscarriage rates by impairing successful implantation of an embryo. Changes in the endometrium or in the blood supply to the uterus may also cause early miscarriage. In addition, increased risk of premature delivery and other pregnancy related problems can be associated with fibroids.
Cancer and Fibroids
The risk of fibroids being malignant is approximately 0.2 percent. This cancer is called leiomyosarcoma and is more likely to occur in a postmenopausal woman. However, if a fibroids begins to grow very rapidly, this may suggest that it has become cancerous and requires careful evaluation and potential removal of the uterus (hysterectomy).
Diagnosis
Ultrasound
Ultrasound, either abdominal or vagina, is a procedure that uses sound waves to create a picture of the pelvic organs. The physician can look at an ultrasound picture to see if fibroids are present. Often, as fibroids vary in size, both transvaginal and transabdominal ultrasound is necessary to visualize them accurately.
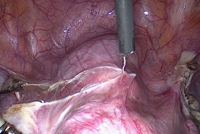
Diagnostic Laparoscopy
Diagnostic laparoscopy can help the physician make a definitive diagnosis and can sometimes be used to remove fibroids. During this procedure, the physician will insert a slender, telescope-like instrument called a laparoscope into the abdominal cavity through a small incision near the navel. The laparoscope is used to look for abnormalities of the internal pelvic organs. This surgery is usually performed on an outpatient basis under general anesthesia and requires one to four days of recovery time. Diagnostic hysteroscopy is sometimes performed at the same time. In a few cases, fibroids can be removed during laparoscopy. This procedure is described later in this booklet.
Diagnostic Hysteroscopy
Diagnostic hysteroscopy is useful to determine the presence of submucous fibroids. This procedure involves the insertion of telescope-like instrument called a hysteroscopy through the vagina and cervix into the uterine cavity to look for abnormalities within the uterine cavity. The surgery can be done under local or general anesthesia. Sometimes the fibroids can be removed through the hysteroscope, but only in the operating room. This procedure is described later in this booklet.
Sonohysterography
With sonohysterography, a small catheter is placed inside the uterus to instill 15-20 cc of fluid during an ultrasound. This improves the physician’s ability to identify submucous fibroids which protrude into or distort the uterine cavity.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) produces a picture by absorbing energy from specific, high-frequency radio waves which can determine if fibroids are present. The created image can define the size and location of the fibroids and can help determine whether or not the fibroids are distorting the uterine cavity. Although MRI is very accurate, it is rarely needed to diagnose the presence of fibroids.
Treatment:
Periodic Examinations
Most of the time, fibroids don’t require treatment. If a woman is not experiencing pain, a pressure sensation, infertility, or excessive bleeding, periodic examinations are generally sufficient to find out if there is a significant change in the fibroid size. This is especially true if she is planning a future pregnancy, when fibroids can grow and affect the pregnancy, or if approaching menopause, when fibroids generally shrink. Even if a woman is infertile, the presence of uterine fibroids is often only coincidental. Surgery to remove the fibroids should be considered only after a through evaluation of other factors which could be causing infertility. In fact, surgery on fibroids can sometimes make the infertility problem worse by creating pelvic adhesions (scar tissue).
Surgical Management of Fibroids
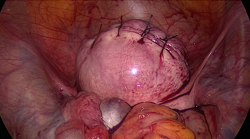
Myomectomy (Surgical Removal of Fibroids)
Fibroids that are large enough to cause significant symptoms or rapidly growing fibroids may require surgery. Removal of only the fibroids, rather than the entire uterus, is called a myomectomy. Myomectomy is most often performed when the woman desires a future pregnancy or when she wishes to retain her uterus. Today, there are several options available for this surgery. In most cases, the size and location of the fibroids will determine the appropriate surgical technique. Small fibroids may be removed through less invasive hysteroscopy or laparoscopy procedures, but large, multiple, or inaccessible fibroids usually require laparotomy for removal. During a laparotomy, the physician will make an incision in the abdominal wall to remove the fibroids from the uterus. It usually takes about four to six weeks for a complete recovery. After a patient has undergone this surgery, a cesarean section may be needed for delivery because the muscular wall of the uterus may be weakened by the removal of many or large fibroids. The physician can make this determination at surgery.
The two major concerns with performing a myomectomy are minimizing blood loss and preventing surgically induced adhesions (scar tissue) that may impair future fertility. In rare cases, uncontrolled bleeding may require a hysterectomy. Sometimes women bank their own blood several weeks before myomectomy in case they might need a blood transfusion. If a woman and her physician decide that myomectomy is the best option, there are other risk factors that will need to be discussed. There is a chance that fibroids will reoccur and require further surgery. Pelvic adhesions may form which can impair fertility by affecting the tubes or ovaries. A laparoscopy can be used to evaluate any postoperative adhesions.
Operative Hysteroscopy
Small submucous fibroids located within the uterine cavity may be removed with operative hysteroscopy. During this procedure, the physician will insert a hysteroscope through the cervix into the uterus. Surgical instruments are then inserted through a channel in the hysteroscope to remove fibroids located within the uterine cavity. Generally, women can return to their normal activities within two days after operative hysteroscopy, and complications are rare.
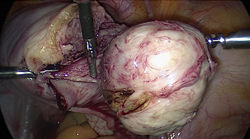
Operative Laparoscopy
In some cases, operative laparoscopy may be used to remove the fibroids if they are located on the outside wall of the uterus. During operative laparoscopy, the physician places a laparoscope into the abdomen through a small incision near the navel and then uses surgical instruments to remove the fibroids. Recovery time is usually two to seven days. A new techmique, called myolysis, in which the fibroid is at least partially, if not completely, destroyed by electrosurgery or other means is being developed.
Hysterectomy
If a woman has large fibroids that are symptomatic, and pregnancy is not desired, a hysterectomy or surgical removal of the uterus may be recommended. A vaginal hysterectomy, which removes the uterus through the vagina, or an abdominal hysterectomy, which requires a laparotomy, may be necessary. Recovery time is usually two to six weeks.
Medical Management of Fibroids:
GnRH analogs can be used to temporarily reduce the size of fibroids. GnRH analogs decrease estrogen levels by stopping the signal from the brain that sends a message to the ovaries to produce estrogen. This can significantly reduce the size of the fibroids. However, when GnRH analog therapy is discontinued, the fibroids usually return to their pretratment size within three to six months. GnRH analogs produce menopausal-like side effects such as hot flashes, vaginal dryness, mood swings, and sometimes bone loss. These medications cannot be used for extended periods of time unless special precautions are taken to prevent bone loss. Primarily, they are used before surgery to reduce uterine fibroid size. In women who have experienced excessive menstrual bleeding and have become anemic, GnRH anlogs may decrease vaginal bleeding. This medication, in combination with iron supplements, may improve anemia, allowing for the possibility of banking blood prior to surgery or reducing the need for a transfusion.
Psychological Aspects:
Women who have uterine fibroids may experience many different feelings. Some women say they feel defective because the condition involves their reproductive organs. It is important to remember that there are many more aspects to femininity and womanhood than one specific body part. Women who have experienced a miscarriage because of fibroids may feel guilty or anxious about future pregnancies. If a woman is faced with the possibility of losing her uterus, she may feel angry and sad, especially if future pregnancy is desired. It is important for a woman to discuss these feeling with her physician so that alternatives to hysterectomy can be discussed and considered. It is also helpful to seek support from family, friends, and support groups.
Summary:
Uterine fibroids are benign masses of smooth muscle tissue in or around the uterine wall. They are commonly found in women during their reproductive years. Fibroids are usually harmless. However, some women experience abnormal uterine bleeding, pain, pressure, miscarriages, or infertility because of fibroids. There is also an extremely small chance that fibroids can develop into cancer. Therefore, it is important that a woman see her doctor at regular intervals to decide if she should undergo surgical removal of the fibroids or have a hysterectomy.
Laparoscopic Hysterectomy:
What is a hysterectomy?
A hysterectomy is a surgical procedure in which the uterus is removed. A total hysterectomy means that the uterus and cervix are removed. A hysterectomy may include removing the ovaries and fallopian tubes-that is called a salpingo-oophorectomy and frequently is performed along with a hysterectomy.
How is it performed?
Historically, hysterectomies have been performed either by making an incision in the abdomen or, if the uterus is not too large, an incision in the top of the vagina-a vaginal hysterectomy. When an incision is made in the abdomen, not only the skin but many other layers need to be cut and to heal. This produces a significant amount of post-operative pain and recovery time. It is actually the healing of the skin and other layers beneath it that accounts for most of the pain women experience after a hysterectomy, not the actual removal of the uterus. A vaginal hysterectomy reduces the pain of recovery, but can only be performed on women who have a relatively small uterus and have no other diseases or prior surgery that may have caused adhesions.
What is a laparoscopic hysterectomy?
Today, there are several surgical approaches that are far less invasive than a total abdominal hysterectomy, which is still widely performed. Using a laparoscope — a slender, fiber-optic tube equipped with a miniature camera, lights and surgical instruments — surgeons have the ability to see inside the abdomen and technical access to the uterus, ovaries and fallopian tubes without having to make a large incision. The surgery is completed utilizing only four tiny abdominal incisions less than one centimeter in length. Even a large uterus can be removed laparoscopically using this technique.

Figure (hysterectomy) Coagulation
of round ligament

Round ligament coagulation
(detaching the connections
of uterus)

Coagulation of left
infundibulopelvic ligament
Seperating the urinary
bladder from uterus
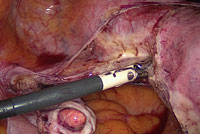
Coagulation of
uterine vessels
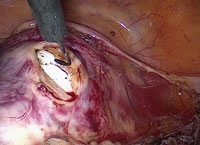
Detaching the
uterus from vagina

Uterus Completely
Detached from Vagina
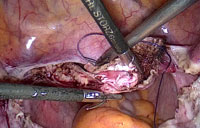
Suturing of vaginal vault
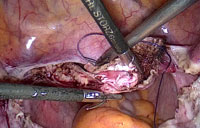
Suturing of vaginal vault
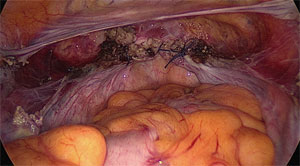 After vault closure
After vault closure What are the advantages of Laparoscopic Hysterectomy?
Who can undergo Laparoscopic Hysterectomy?
Usually all the patients who have been advised for abdominal hysterectomy can undergo laparoscopic hysterectomy.
Can a person who has undergone operations in the past go in for laparoscopic hysterectomy?
Yes, a patient who has undergone operations in the past can undergo this procedure and if there are adhesions because of previous operations, they can be removed along with the laparoscopic hysterectomy, in the same sitting.
Can associated ovarian, tubal or uterine disease all these be treated in the same operation laparoscopically?
Yes, it is very much possible to treat/remove the ovaries and tubes while carrying out laparoscopic hysterectomy.
Do I need any special investigations for laparoscopic hysterectomy?
The usual routine tests are required as for any other operative procedure and no special investigation is required for laparoscopic hysterectomy.
Can a person having disease like diabetes or high blood pressure undergo this procedure?
Yes, after controlling the diabetes and high blood pressure, a person can undergo this procedure, and in fact the advantages of lesser chances of infection and early recovery are much beneficial for them.
Where should one get the laparoscopic hysterectomy done?
It is an advanced laparoscopic surgery procedure, and it’s always advisable to get it done in an advanced care institution, where the whole set of equipment is present along with its complete backup facilities.
Do I have to get admitted a day before the surgery?
If you are fully investigated and have undergone a pre-anaesthetic checkup, you can get admitted the morning of the operation.
Under what type of anaesthesia is it carried out?
This procedure is carried out under general anaesthesia.
After how many days can I go back home after the surgery?
On an average the total hospital stay is for 24-48 hours, after which you can go back home.
What are the usual precautions I have to take after I reach home?
On an average, two hours after lunch and eight hours rest after dinner is what is usually recommended. You can climb stairs for two to three floors slowly, walk half to one km slowly and carry out sedentary work at home without much difficulty. One can have daily bath.
When do I see the doctor again after the operation?
Routinely, the patient is called after 4 weeks for an internal checkup.
When can I resume my normal activity / go back to work?
After one week, you can resume normal activity like walking, cooking, driving, sitting in front of the computers for 4-6 hrs etc. Intercourse, strenuous exercise, lifting of heavy weights, swimming etc. has to be avoided for a period of six weeks.
Questions you may ask …
Q. Will hysterectomy affect my sex life?
No. Hysterectomy does not make a women sexually mutilated and undesirable it does not shorten her Vagina so that sexual intercourse is impossible or potentially dangerous. In most cases when the womb is removed the vagina is cut at its uppermost end, and the cervix no longer projects into it so if anything the vagina is a little longer after the operation. In rare cases the cervix is left when the surgeon removes the section of the womb above it. In such a case there is no alternation at all to the vagina.
Q. Must I take some medication for the rest of my life?
No, unless both ovaries are removed. Then you will need to take only the oestrogen tablets, to replace natural hormones – and these only for a limited time.
Q. Will suffer a personality change?
This is really up to you. If you convince yourself you will be changed nothing will prevent you from becoming a chronic neurotic. But the operation will not cause it.
Q. How soon will I be able to return to normal duties?
As with any other major surgery It is advisable to take things quietly for 2 weeks and gradually Increase activity rather than rush into it. Your doctor will advice about the length of time needed for convalescence – usually 3-4 weeks.
Q. Will be semi –invalid for the rest of my life?
No you will no doubt feel healthier than before the operation as the complaint for which it has been advised will be cured.
Q. Would an outsider know I had a hysterectomy?
There will be no visible signs. Many of the women you pass daily in the street, or work with have had the same kind of operation. If you or your husband have any further questions or fears you would like to allay, talk it over with your doctor. He – not an uninformed relative or friend – is qualified to advice.
Q. But will sex be as satisfying to me after the operation?
There will be no difference in sexual desire or satisfaction after the hysterectomy. In fact where there has been some fear of pregnancy, when all possibility of pregnancy has been removed a woman’s sexual desire or satisfaction after the hysterectomy. In fact where there has been some fear of pregnancy when allpossibility of pregnancy has been removed a woman’s sexual desires and reponse may increase.
Q. will still be able to reach an orgasm or “climax” during intercourse?
Yes removal of the womb has no effect on this.
Q. Will my husband be able to feel to any physical change in my body, when we have sexual intercourse?
No unless he was told a man would not know a woman had undergone this type of surgery.
Q. How soon after the operation should my husband and I resume normal sexual relations?
Once the top of the vagina has healed strongly, which takes about six weeks sexual intercourse can be resumed safely and with normal satisfaction.
Q. Will I become fat?
Only if you sit about and eat too much instead of carrying on normal activities. Woman who grows fat after any surgery usually do so because during convalescence a pattern of over eating and under exercising is set and this begins a habit difficult to break.
Q. Will I become hairy or develop male characteristics?
No the womb does not produce any hormones – the ovaries do this – so removal of the womb will make no difference to hormone balance.
Q. Will I go through an immediate “change of life”?
Only if both ovaries are completely removed in which case the oestrogen tablets you will be given will minimize or completely relieve symptoms.
Discharge Guidelines:
Discharge guidelines for endoscopic surgery
Discharge guidelines for hysterectomy: