Services:



Gynaecology and Obstetric Services:
Dr. Dasmahapatra is personally familiar with many of the concerns and issues women and couples face. His years of clinical experience, both in the india and abroad, have deepened his understanding further and have also allowed him insight into other cultures and customs. He fervently believes that each one of his patients is an individual with individual circumstances and treatment needs, and these he aims to address with a sympathetic ear and an open mind in his practice.
• Dr. Sankar Dasmahapatra :: Consultant Gynaecologist and Obstetrician provides consultations on:
1) Abnormal Menstrual Bleeding:
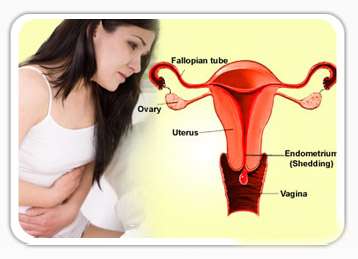 Irregular menstrual bleeding or heavy menstrual bleeding or a combination of both may characterize abnormal menstruation.
Irregular menstrual bleeding or heavy menstrual bleeding or a combination of both may characterize abnormal menstruation.
World wide up to 20% of women will suffer from heavy menstrual bleeding (HMB) at some point in their lives. It accounts for 12% of referral to gynaecology outpatient departments.
Historically up to 60% of women would end up with a hysterectomy within 5 years of referral but there are now a number of effective alternative ways to manage HMB without recourse to hysterectomy.
The holistic approach to the management of HMB is important as it depends on a woman’s symptoms as well as her circumstance, whether her family is complete or whether fertility is still desired. A woman should not be compelled to remove her womb if she doesn’t want to, and on the other hand she shouldn’t be forced to keep it if it is detrimental to her quality of life. This course of management is underpinned by NICE (National Institute of Clinical Excellence) guidelines in the UK.
In the absence of any overt pathology it is possible to manage HMB with medication in some cases hormones will not be required. The next step of management would then be hormonal manipulation. This may be in the form of tablets or the use of the Mirena™(a small device that is inserted in the womb and gives off low dose hormones) and if all this fails surgery may be required.
Even when surgery is required hysterectomy is not the starting point measures to remove or destroy the lining of the womb are effective treatments in up to 70% of women.
For women who do require hysterectomy tradition open surgery should not be and is no longer the norm. It is now possible to carry out most hysterectomies though minimal access techniques, sometimes irrespective of the size of the uterus.
The questions women should always ask her gynaecologist should always include: whether she is able to have her hysterectomy by minimal access techniques and if not why? Whether she needs to have her cervix removed during the hysterectomy and whether she needs to have her ovaries removed.
2) Abnormal Cervical Smears
Cervical screening in the UK has been a success in screening to prevent cervical cancer, about 4.4 million women are screened in the UK each year. Screening starts at the age of 25 and goes on till 65 years provided the last smears have been normal.
3) Complications of Early Pregnancy (Miscarriage):
 Miscarriage presents with pain and or bleeding in early pregnancy, after missing a menstrual period. Unfortunately miscarriage is not uncommon. 1 in 8 pregnancies will miscarry. Once a woman has a positive pregnancy test within the first 3 months there is a 20% chance that she might miscarry. Between 6 and 9 weeks the risk falls to about 4% and after 9 weeks to 3% in the first trimester. The risk of miscarriage increases after a third miscarriage and with age.
Miscarriage presents with pain and or bleeding in early pregnancy, after missing a menstrual period. Unfortunately miscarriage is not uncommon. 1 in 8 pregnancies will miscarry. Once a woman has a positive pregnancy test within the first 3 months there is a 20% chance that she might miscarry. Between 6 and 9 weeks the risk falls to about 4% and after 9 weeks to 3% in the first trimester. The risk of miscarriage increases after a third miscarriage and with age.
From the early 1990s the management of miscarriage has changed in the United Kingdom with all units that care for women with complications of early pregnancy having dedicated areas and dedicated staff, who are experienced and versed in the management of complications of early pregnancy (Early pregnancy assessment units). These allow women continuity of care, provide counseling and support, and allow all tests and therapies to be carried out in dedicated areas, and avoid unnecessary and repeated internal examinations.
Once a woman experiences pain and bleeding in early pregnancy she will be referred to one of these units in her local area.
Miscarriages are usually defined as:
On arrival at the EPAU the objective would be to try and determine what type of miscarriage is taking place. A pregnancy test is usually organised and depending on how many weeks pregnant the woman is an ultrasound scan is then arranged. If the fetal heart is seen beating on the ultrasound scan she is reassured and in most cases sent home. If any of the above types of miscarriages is identified management choices are:
Traditionally surgical management was the only therapy offered but depending on a woman’s symptoms and her preference she may be offered expectant or medical management. There are certain criteria that need to be met for safety and efficacy of the first 2 methods of management.
Whatever management is offered women are offered counseling for the emotional implications of miscarriage and how if necessary to manage future pregnancy.
4) Endometriosis
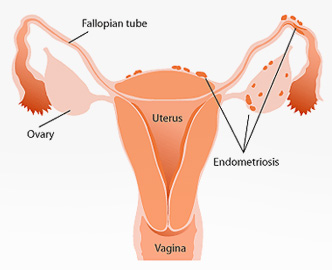 Endometriosis is a chronic condition where endometrium (this is the lining of the inside of the womb) is found outside the womb. It can be responsible for pelvic pain, pain during intercourse and in some women infertility.
Endometriosis is a chronic condition where endometrium (this is the lining of the inside of the womb) is found outside the womb. It can be responsible for pelvic pain, pain during intercourse and in some women infertility.
5) Ectopic Pregnancy:
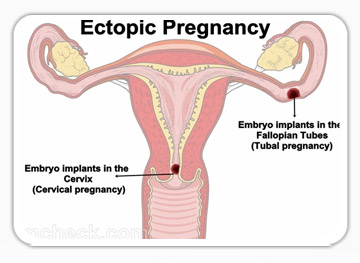 Ectopic pregnancy is a pregnancy that is situated outside the womb. The most common site is the fallopian tube. It is a potentially life-threatening condition and occurs in about 1:100 pregnancies.
Ectopic pregnancy is a pregnancy that is situated outside the womb. The most common site is the fallopian tube. It is a potentially life-threatening condition and occurs in about 1:100 pregnancies.
Common symptoms are abdominal pain and bleeding after missing a menstrual period, with a positive pregnancy test.
Risk factors for ectopic pregnancy include: previous ectopic pregnancy, previous tubal surgery, previous pelvic infection, current IUCD use. Though most women who present with ectopic pregnancy will have none of these symptoms.
Ectopic pregnancies are usually diagnosed on the basis of symptoms and a blood test which measures the amount of Beta-HCG which is a pregnancy related hormone, and an ultrasound scan.
For the majority of women it is possible to make a diagnosis after initial investigation but in some women the results of investigations may be inconclusive and follow up scans and blood tests may be necessary.
Once the diagnosis is established women may be given a choice of how they would prefer their ectopic pregnancy to be managed. The choice is sometimes limited however by symptoms and the results of investigations.
Choices include:
1. Conservative, Expectant management, where women are kept under surveillance until the pregnancy resolves by itself.
2. Medical management: this is where a drug called Methotrexate is given to “kill” the rapidly dividing ectopic pregnancy cells. This modality of treatment depends on Beta-HCG levels and scan findings. The pregnancy may also take some time to resolve.
3. Surgical management: the majority of women who have ectopic pregnancies are managed by surgery. Traditionally surgery used to be by conventional open surgery but now it is possible to manage nearly if not all ectopic pregnancies by means of laparoscopic surgery.
Despite evidence that laparoscopic surgery is superior to conventional surgery unfortunately not all women with this condition even if stable are managed by laparoscopic surgery with figures ranging from between 39% and 89% in india
Dr dasmahapatr has wide knowledge and research interest in this area. Under his direction all (100%) women who are haemodynamically stable have laparoscopic surgery for the management of ectopic pregnancy when this is required. Even in haemodynamically unstable women 85% are managed by means of laparoscopic surgery by a highly skilled team of surgeons, nurses and theatre.
Even for the rarer ectopic pregnancies Dasmahapatra has demonstrated that laparoscopic surgery is feasible.